Diabetic Eye Disease & Management
Diabetic Retinopathy
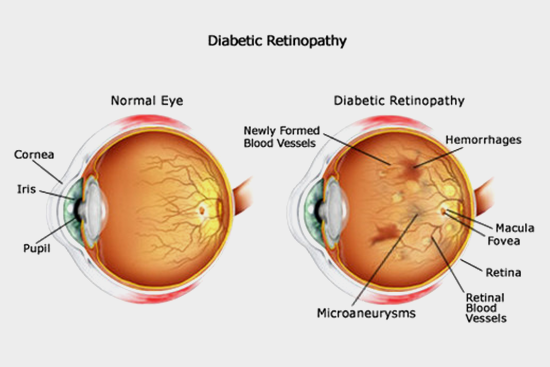
Diabetic retinopathy is caused by changes in the blood vessels of the retina. When these blood vessels are damaged, they leak blood and grow fragile new blood vessels. These changes can cause blurry vision and hemorrhages into your eye or if untreated can result in retinal detachment.
Diabetic retinopathy is the most common diabetic eye disease and leading cause of blindness.
Causes of Diabetic retinopathy
People with uncontrolled diabetes are 25 times more at risk than the general population. With regular, proper eye care and treatment when necessary the incidence of severe vision loss can be reduced. If you have diabetes your ophthalmologists can help to prevent serious vision problems.
Risk factors (add in order)
- Poorly controlled diabetes
- High blood pressure
- Long term duration of diabetes
- Elevated blood cholesterol levels
Symptoms
- Blurred vision
- Sudden loss of vision in one eye
- Seeing rings around lights
- Dark spots or flashing lights
Diagnosis of Diabetic Retinopathy
Indirect ophthalmoscope: Dilated retinal examination that is to check inside the eye with an ophthalmoscope.
Diabetic Macular Edema
Macular Edema is a condition where the retinal blood vessels develop tiny leaks. When this occurs, blood and fluid leak from the retinal blood vessels and fatty material (called exudates) is deposited in the retina. This causes swelling of the retina and so it is called as diabetic macular edema .this causes blurry vision.
Proliferative Diabetic Retinopathy
It refers to the changes that occur when new abnormal blood vessels begin to grow on the surface of your retina. This abnormal growth is called neovascularization. These blood vessels have weaker walls and may break and bleed, or cause scar or tissue to grow that can pull retina away from the back of your eye. When your retina is pulled away it is called as retinal detachment, and if kept untreated it may cause severe vision loss, including blindness.
Leaking blood can cloud the vitreous-the clear, jelly like substance that fills the back of the eye-and block the light passing through the pupil to the retina, causing blurry and distorted images.
Diagnosis
Macular edema and proliferative diabetic retinopathy can be assessed through dilated eye examination.
Fluorescein Angiography: to rule out bleeding damaged blood vessels and abnormal new vessels of the retina.
OCT: macular edema can be assessed using OCT. macular edema is noted when areas of your retina are shown to contain spaces filled with fluid.
Treatment
In mild cases, treatment for diabetic retinopathy is not necessary. Regular eye exams are critical for monitoring progression of the disease.
In advance cases treatment is recommended to stop the damage of diabetic retinopathy, prevent vision loss, and potentially restore vision.
Treatment options include,
- Anti VEGF therapy: Anti VEGF therapy involves the injection of the medication into the back of the eye. The medication is an antibody designed to bind to and remove the excess VEGF (vascular endothelial growth factor) present in the eye that is causing the disease state.
- Laser surgery: Laser surgery is helpful in treating diabetic retinopathy. To reduce macular edema, a laser is focused on the damaged retina to seal leaking retinal vessels. For abnormal blood vessels growth (neovascularization), the laser treatments are delivered over the peripheral retina.
- Vitrectomy: Vitrectomy may be recommended in advanced proliferative diabetic retinopathy. During this microsurgery procedure, the blood filled vitreous is removed and replaced with a clear solution.
Preventive Tips
- Keep blood sugar level within normal limits
- Monitor blood pressure and keep it under control
- Exercise regularly
- Maintain healthy diet
- Quit smoking
- Follow your doctor's instructions
- Regular eye checkups